In a pharmaceutical landscape crowded with me-too medications and generic alternatives, even well-know pharma companies find it increasingly challenging to break through the competitive clutter. Given the sea of sameness, crafting just the right messaging can play a make-or-break role in differentiating a drug and capturing more mindshare.
Category: Healthcare
Brands with Personality
When is water more than just water? Ask the billion-dollar beverage brand Liquid Death. Between 2022 and 2023, Liquid Death’s retail sales grew 100% from $110 million to $263 million. The brand’s valuation is now double what it was worth in 2022. This warp-speed trajectory is particularly remarkable when you consider what Liquid Death sells: water.
Post-Treatment Patient Studies
In our previous post, “Surviving Survival: Unmooring After the Patient Journey,” we explored the myriad challenges patients and their families face after finishing treatment for a medical condition. We also encouraged healthcare and pharmaceutical companies — along with the market researchers who work with them — to include these post-treatment patients in qualitative research studies.
Surviving Survival: Patient Unmooring after the Patient Journey
Bonnie Dibling, CEO & Lead Healthcare Researcher
March 25, 2024
Over the span of my 25-year career in qualitative research, I’ve had the privilege of collaborating with healthcare and pharmaceutical innovators whose breakthrough treatments have helped countless patients struggling with serious and chronic conditions. In this work, I’ve seen first-hand the dedication, compassion, and drive of medical professionals and researchers as they strive to find cures for often devastating diseases.
I’ve also had the privilege of talking with hundreds of patients, family members, and caregivers for whom these innovative treatments are meant. Following several recent projects we completed with a biotech company developing a novel treatment for certain chronic diseases, I’ve been thinking more and more about what happens to these patients after their treatment is finished.
Clearly, finding out that the treatment worked and the patient is now disease-free are causes for celebration and relief. But for many patients as well as their loved ones, the end of a long and difficult treatment can trigger the start of an emotional struggle. And unlike the original disease, this psychological aftereffect often goes untreated.
Abandoned, Anxious, and Alone
People who have been successfully treated for cancer, autoimmune disorders, heart attacks, strokes, chronic diseases, and any number of serious conditions can experience what I’ve come to think of a “patient unmooring.” Given a clean bill of health, these patients are in essence cut loose from their doctor and care team, and told to go forth and live their lives. Besides the annual follow-up, there are no more doctor’s visits, no more therapy appointments, no more competent medical professionals guiding them. This can leave patients feeling abandoned.
The disease may be gone, but the trauma left by the patient’s medical experience is still very much present. This trauma can manifest itself in multiple ways. Fearful that the disease will return, patients may start to catastrophize. Feelings of anxiety and depression creep in, overshadowing any joy that comes with a clean scan or encouraging lab result.
Studies reported by the Lancet Oncology, for instance, found that long-term cancer survivors and their spouses experience higher incidents of anxiety than participants in healthy controls. A 2023 study published the General Hospital Psychiatry journal showed a high prevalence of anxiety and depression in survivors of cardiac arrest (up to 24%), with anxiety symptoms persisting for one year or more.
In studies of COVID-19 patients who had been treated in the ICU, feelings of anxiety and depression in these patients increased over time and remained high even 12 months after discharge. According to the findings, 42% of these patients experienced long-term anxiety and 40% suffered from lingering depression.
Patients who are unable to be overjoyed or grateful for their recovery may also have feelings of guilt and shame. It can seem like everyone around them — from providers to loved ones — expects the patient to pick up right where they left off before they got sick. This can lead to feelings of isolation, as patients are unable to share what they’re going through with others.
Medical Trauma After Treatment
Indeed, the post-treatment experience of some patients falls within the definition of post-traumatic stress disorder (PTSD) — a health condition triggered by a terrifying event. The International Society for Traumatic Stress Studies reports that 20% to 30% of people who receive intensive care experience PTSD symptoms after being discharged. Studies reported by Frontiers in Psychology also show a high incidence of PTSD for patients who have been in vulnerable medical situations, including childbirth.
Often referred to as medical trauma, medically related PTSD can result from a patient’s exposure to pain, injury, serious illness, and medical procedures. Lengthy, complex, and/or painful or intrusive treatments coupled with uncertainty around outcomes certainly fall within the medical-trauma category. Symptoms of medical trauma run the gamut and can include numbness, disassociation, panic attacks, feelings of rage or shame, substance use, eating disorders, self-harm, compulsive behaviors, sleep problems, as well as anxiety and depression. I’ve heard patients describing many of these symptoms when speaking about their post-treatment experiences.
While trying to navigate these psychological hurdles after completing their treatment, patients have no care team or doctor to turn to, and no tools or resources to guide them. Which leads to the question: Why not? And a follow-up question: How can we change this?
Meeting the Challenge with Research
Here is my challenge to the healthcare, medical, and pharmaceutical community, including the qual researchers who help them better understand patients (I count myself among those). In the noble quest to develop and launch breakthrough treatments for chronic and serious medical conditions, healthcare innovators must also consider what happens after the treatment.
What can be done to avoid patient unmooring? How can we keep patients connected to compassionate and competent medical professionals trained to help them understand and manage the physical, mental, and emotional impact of the trauma they’ve lived through?
Understandably, the focus of novel treatments has long been on the clinical ramifications for survival. Cure the disease so that the patient can live. Let’s expand the focus to include what that life is like once the treatment is finished and the disease has been vanquished. In our qual research, let’s learn more about the needs of these patients and their families post-treatment and use those insights to inform innovative strategies to support their mental wellbeing.
A few of these strategies have already been tried and tested with encouraging results. The non-profit Regenstrief Institute and the Indiana University Melvin and Bren Simon Comprehensive Cancer Center recently co-launched a pilot study for breast cancer survivors incorporating acceptance and commitment therapy (ACT). After receiving 6 weeks of group-based ACT, women participating in the study developed better skills and tools to help them cope with distress and anxiety. Six months after completing the program, the women reported a significant reduction in their fear of cancer recurrence as well as fewer symptoms of anxiety and depression.
Another pilot program launched by the Arizona State University Edson College of Nursing and Health Innovation explored the benefits of digital storytelling to help patients who had undergone hematopoietic stem cell transplantation (HSCT) as well as their caregivers. Participants completed a digital storytelling workshop, then together they watched the digital stories they had created about their personal experiences. Researchers are now assessing whether these shared stories helped the HSCT treatment survivors and their caregivers cope with psychosocial distress and isolation.
While these pilot programs are a promising start, there are significantly more untapped opportunities to explore post-treatment patient care focused on emotional and mental wellbeing. As mission-driven innovators seeking to improve lives, healthcare and pharmaceutical companies also have the opportunity to lead the charge in this type of research.
As qual researchers who specialize in healthcare, we would welcome participating in these studies. And we think patients would as well.
Transformative Insight: Helping a Biotech Innovator Find Their Target Audience
Patients with chronic conditions often live with near-constant pain and discomfort, compounded by long-term treatments that come with unpleasant side effects. So when a biotechnology company discovered that an existing treatment could be adapted to treat and possibly even cure a select group of non-malignant chronic diseases, they knew that had the potential for a breakthrough new therapy. They also knew they needed to learn more about the medical professionals who might one day be offering this transformative treatment to their own patients.
After searching for a research firm, the company connected with Thinkpiece and knew they had found a kindred partner — one who is just as energized about the potentially life-changing treatment they were developing. Our healthcare research team offered exactly the multi-faceted experience the client was looking for: first-hand healthcare knowledge as former clinicians-turned-researchers combined with B2B expertise.
A Partnership Built on Shared Passion
We jumped at the opportunity to collaborate with this innovative biotech company led by a brilliant team of doctors and scientists. As this was the company’s first foray into qualitative market research, the client was excited to be part of the process and open to learning as much as possible about their audience. We were equally excited to join the client’s journey at the early stages of development and discovery, where our research could have the greatest impact.
In the first year of our partnership with the client, our research focused on answering two key questions: does it make sense to pursue this treatment for chronic diseases, and if so, what does it mean for the future direction of the company? For the initial studies, we found and recruited doctors with a specific specialty to glean their level of interest in offering this therapy to their patients, and how doing so might affect their practice. The response we received confirmed what the client suspected, while also revealing unexpected truths.
Finding Answers and Direction
Our first research studies clearly identified a need for a novel treatment like the one our client is developing, and excitement on the part of doctors. We also discovered that the doctors we interviewed were hesitant about the prospect of delivering this complex new treatment to their patients through their own practices. Based on these findings, we uncovered that delivery of the therapy would likely require collaboration and coordination with a highly specialized healthcare team.
These initial studies opened the door to additional research into the types of practices and specialties that would be more likely to have the competencies and willingness to deliver this highly complicated treatment. For these follow-up studies, we were tasked with finding a very specific type of respondent with unique management responsibilities within a healthcare organization. Our resourceful field manager was able to recruit the right respondents to meet the criteria and get us the answers we needed.
The client additionally credits our team with having the clinical experience to converse comfortably and confidently with high-level medical professionals, know which questions and follow-up questions to ask, and expose a more meaningful layer of insight. Building on our previous familiarity with this particular field of therapy, we were able to quickly grasp the highly technical and complicated nature of the treatment and dive into the studies quickly.
(Re)usable Reports
The studies we’ve completed with the client to date have provided the leadership team with the foundational insight to steer the company’s strategic direction and future research. By bringing Thinkpiece into the process early in the company’s development, the client has been able to avoid incorrect assumptions and make more informed decisions about where to take their treatment.
The client has additionally been able to leverage the insights from the reports we generated for external presentations, including with investor audiences, and plans to leverage the insight for key decision-making moving forward. We look forward to continuing our collaboration with this innovative, mission-driven company as they bring their breakthrough treatment to market and in the hands of medical professionals who will use it to improve millions of patients’ lives.
Explore Thinkpiece’s healthcare research experience here.
Inflation, Trauma, and the Importance of Asking the Right Questions
“Trauma” can easily be used to describe nearly every aspect of the COVID-19 pandemic. From the tragic loss of life and lingering health issues to significant shifts in social discourse, political systems, and the global economy, the world is traumatized. And today, as both people and businesses navigated the ebb and flow of changing mandates and regulations, we’re all watching as inflation — a key aftereffect of trauma — grows.
This steady increase is concerning but is nothing new. The United States saw inflation in the late 1940s as the country transitioned out of wartime production from World War II. We felt it again in the 1970s (oil shocks) and more recently around 2008 (rising gas prices). Inflation is the economic result of national traumas, such as war, depressions, oil embargoes, and, as we’re all learning, pandemics. You could argue the current inflation is different. It’s global, its trigger is a microscopic threat, and there’s a significant lack of unity regarding how to navigate the turmoil. You could also argue that it’s not nearly as bad as those prior examples. However, these arguments are nothing more than speculation.
That’s not what you need. It’s not what customers want. And waiting for answers isn’t going to help. So, rather than playing a guessing game, it’s time to accept what we don’t know and start asking the questions that matter (hint: this involves turning to your customers).
Today’s Inflation is an Educated Guessing Game
Predictions from leading economists point to both continued inflation and dropping rates, with compelling arguments on both sides.
Inflation will last a while because…
- Gross Domestic Product (GDP) is slow and cannot mitigate inflationary forces.
- Emotions are low. The “Misery Index” — currently at 10.8% — spiked for the first time since the oil embargo.
- Housing prices are rising for renters and owners.
Or inflation may be transitory because…
- The Consumer Price Index (CPI) is calculated in arrears, uses outdated measurement methods, and undercounts online expenditure.
- The underlying reason for inflation — too much money chasing too few goods — will shrink as the global supply chain heals.
- Technological advances are a deflationary force, and innovation in the tech sector has not slowed.
But here’s the thing: Every historical episode is nuanced. We don’t have a 1:1 comparison. Yes, it’s important to predict and plan, but knowing what your customers need and want from you now is more important.
Stop Waiting for Answers, Start Asking the Right Questions
Definitive answers are unlikely, if not impossible, so start focusing on definitive action. Start identifying what you need to understand about your customers and your place in their world. For this to be effective, you must think big and small and look beyond the numbers. Consumer (B2B and B2C) behaviors are a direct result of how we feel, and the messages and information we received affect those feelings. First, start by understanding your customers’ overall next steps and behaviors:
- In a post-COVID environment, what consumer behaviors are going to be influenced by inflation?
- How does that differ from pre-COVID inflationary consumer behavior?
- What commonalities exist between post-COVID and pre-COVID inflationary consumer behavior?
Then focus on what you can do to help regardless of which inflation prediction comes true:
- What messages reassure skittish consumers to keep them supporting your business?
- In the face of uncertainty, what does your business offer that can help?
- What more do they need from you given the changing landscape?
We think of this as the transition from “what if…” to “so what?”. In other words, it’s important to imagine and plan for both inflation scenarios, but then you need to stop asking “what if…” and start asking “so what are we going to do now?” The only way to answer that question is to listen to your customers.
Sure, some of the answers may change in a year or six months or even less. But predictions on the economy will change, too, and there’s not much you can do about that other than watch, wait, speculate, and worry. We prefer action, especially when all you have to do is ask.
Patient Psychology
Healthcare.
Bonnie’s extensive clinical background helps her engage with healthcare professionals as an equal and patients as an understanding peer. Learn more about Bonnie’s commitment to qualitative research.
Understand.
A global pharmaceutical company launched a novel product to manage a chronic pain condition, but prescription rates were lower than projected. The client had several hypotheses regarding prescription, with two leading theories emerging:
Medication cost was prohibitive/insurance coverage was problematic
Physicians awareness was low and/or they were not mentioning it to eligible patients
However, research into the discrepancy between projection and initial uptake hadn’t been conducted. The client didn’t want to move forward with marketing or outreach initiatives without understanding the underlying issues.
Design.
We needed understand the psychological state of the patient before assessing factors which may or may not compel them to consider the medication. With this emotional foundation, we could move on to explore the affects of potential tactical barriers such as cost.
To accomplish this, a robust qualitative study was needed. A nationwide sample of patients was recruited, all of whom had awareness of the medication, but most of whom chose to reject taking it.
To offer the client usable insights, we knew we’d also need to understand the prevalence of the barriers—emotional and tactical—identified in the qualitative study. To accomplish this, a quantitative study was designed for use after the qualitative research was complete.
Execute.
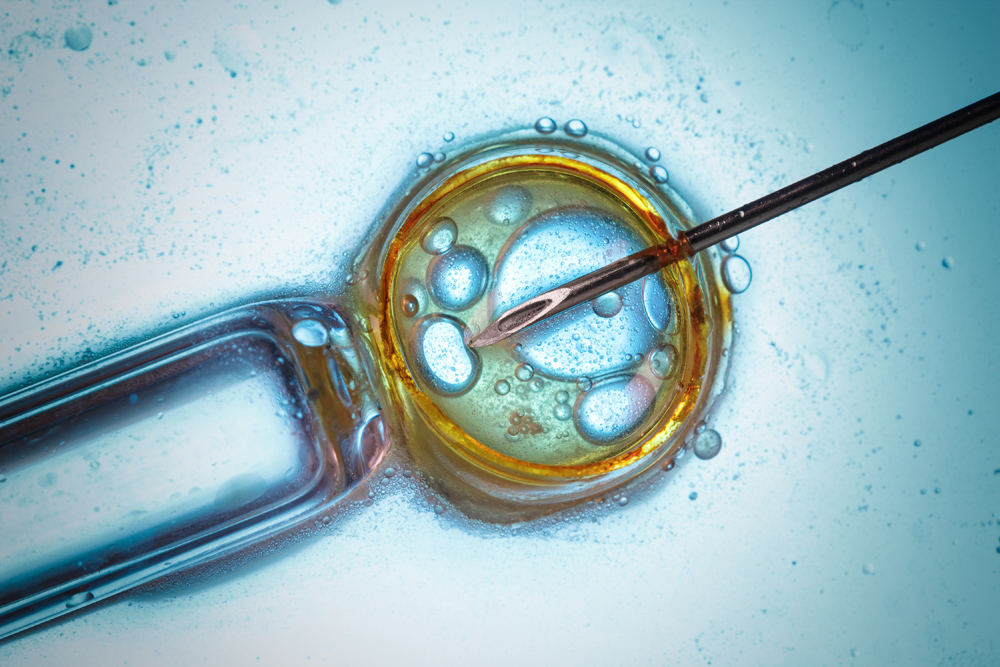
Through conversations with patients, we identified complicated and deeply rooted psychological reasons for rejecting the medication. Very few patients hesitate because of any practical reasons such as cost. Rather, patients wait until they reach their own personal “breaking point” with their pain before accepting the need for the medication. The condition and treatment affect intimate aspects of a patient’s life, including libido and reproduction, so many choose to “suffer” with the pain. Similarly, many belive the potential for side effects are not worth the risk.
Physicians consistently offer the medication, but very few advocate for it or provide adequate guidance. They leave the decision entirely up to the patient, causing them to feel overwhelmed and frozen not only by the disease, but also how to move forward with it.
Analyze & Advise.
Increasing prescription rates is about more than overcoming tactical barriers. Rationally, patients understand the risks and rewards of medication but are not compelled to pursue treatment due to the personal nature of the disease and the emotion behind treatment decisions. Though every patient experience is unique, the qualitative research revealed common threads while the the quantitative portion of the study allowed us to better prioritize action by highlighting the prevelance of these experiences.
To increase patient uptake of the medication, several key recommendations were made to the client:
Revamp advertising to convey the patient’s worthiness of having pain relief – that they do not have to live with pain any longer. Bring their breaking point to them.
Reassure patients about side effects. Pain relief and improved quality of life are worth the risk of usually minor side effects. Make the risk/benefit case clear and easy to understand.
Develop a campaign to turn prescribing physicians into advocates. Help them see how the medication will improve patients’ lives.